Nanomedicine
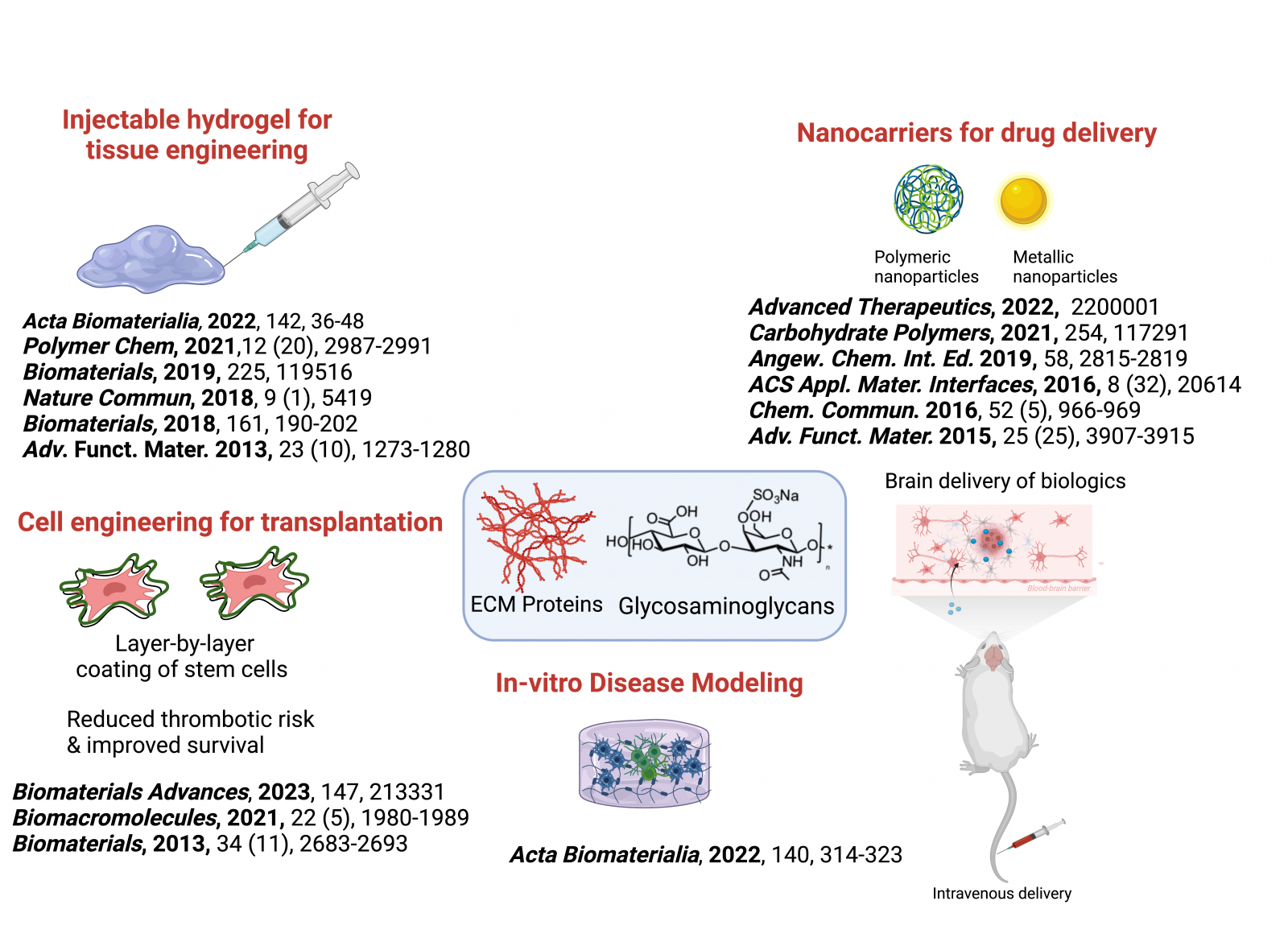
Nanotechnology has made significant contributions to the field of medicine by overcoming major limitations in drug delivery, diagnosis, and imaging. However, the successful translation of these advances to clinical use still faces several challenges. These include poor half-life in blood, immune rejection and sequestration in the liver or fast elimination from the kidneys, limited shelf-life, limited encapsulation capacity, and off-target effects. To address these challenges, our research group is designing functional nanocarriers that can overcome these obstacles.
We are exploiting the intrinsic capability of glycosaminoglycans to evade immune rejection and promote targeted delivery to CD44 overexpressing solid tumors or EGFR overexpressing cancers. Recently, we have developed diverse polymeric nanocarriers for targeted drug delivery, plasmid DNA, and siRNA delivery. A major focus of our research is to deliver drugs to the brain for the treatment of neurological diseases. We have discovered that heparin-based nanoparticles can penetrate the blood-brain barrier and target glioma cells. Our goal is to expand the portfolio of biologics that can be delivered to the brain. Although our current focus is on glioma, we are developing nanoplatforms for other neurological applications. We are also developing polymer-coated liposomes and micelles for other tumors such as prostate cancer, colorectal cancers, and breast cancers.
In summary, our group is actively working to design and develop nanocarriers that can overcome the challenges of drug delivery and bring the promise of nanomedicine to clinical use. Our research focuses on creating targeted and effective therapies for various diseases, including neurological diseases and cancer.
Key Publications: Advanced Therapeutics, 2022, 2200001, Biomaterials Science, 2021, 9 (11), 3939-3944; Biomacromolecules, 2021, 22 (5), 1980-1989; Carbohydrate Pol., 254, 2021, 117291; Cancers, 2021, 13 (16), 4032; Biomaterial Sciences, 2019, (8), 1, 302-320; Scientific Reports, 2017, 7, 10355; ACS Applied Materials and Interface, 2016, 8, 20614–20624; Chem Commun 2016, 52, 966-969
Designing injectable hydrogels for tissue engineering and disease modeling
Developing new crosslinking chemistry for designing ECM mimetic hydrogels: Using the transformative power of organic chemistry and polymer chemistry, we develop new biofriendly crosslinking chemistry to tailor functional hydrogels. We discovered carbodihydrazide based hydrazone chemistry that displayed exceptional stability under physiological pH (Advanced Functional Materials, 2013, 23 (10), 1273-1280) and could be adopted as an alternative to click chemistry. We are currently developing novel protein-glycosamioglycan gels that could be utilized to tailor new functional materials.
Key Publications: Biomaterial Sciences, 2022, 10, 6399-6412; Nature Materials 2021, 20 (2), 250-259; Polymer Chem, 2021,12 (20), 2987-2991; ACS Applied Materials and Interface, 2019, 11 (41), 38232-38239; Polymer Chem., 2019 10, 4322-4327.
Tissue Engineering: Scaffold design is a critical component of tissue engineering. The requirements for 3D scaffolds tailored for stem cell delivery differ from those needed for delivering growth factors or small molecule drugs. In addition, the design of bioinks for 3D bioprinting requires a different set of parameters. To engineer 3D scaffolds using extracellular matrix (ECM) polymers such as hyaluronic acid, chondroitin sulfate, and collagen, we prioritize the biological outcome of the tissue-engineered construct. We have developed growth factor sequestering hydrogels for BMP-2 delivery in bone tissue engineering, tissue adhesive gels for the delivery of limbal stem cells and adipose stem cells in corneal epithelium and stroma regeneration, conductive collagen-hyaluronan gels for cardiac tissue engineering, and immunomodulatory hydrogels that polarize macrophages to an immunosuppressive phenotype for other tissue engineering applications. Additionally, we have recently developed a brain-mimetic hydrogel for the differentiation of neuronal cells. Therefore, our aim is to create gels with optimal physiochemical and viscoelastic properties that meet the specific tissue requirements for various target tissues.
Key publications: Biofabrications, 2023, 15 (1), 015020; Acta Biomaterialia 2022, 140, 314-323; Adv. Healthcare Materials. 2021, 2002058; Biomaterials, 2019, 225, 119516; Biomaterial Sciences, 2019, 7, 3906-3917; Biomacromolecules, 2019, 20, 1412–1420; Nature Communications, 2018, 9, 4049
Designing complex immune in-vitro models and tumor microenvironment: We also develop advanced in-vitro models by creating complex immune models that replicate the characteristics of diseased tissues and tumor microenvironments. This involves developing extracellular matrix mimetic 3D matrices that mimic the composition and mechanical properties of human tissues and are cultured with human immune cells and the target tissue cells. These 3D models simulate an organotypic human tissue microenvironment, enabling us to better understand the underlying biology of various inflammatory diseases, such as neuroinflammation, cancer, and diabetic wound healing. They also provide valuable opportunities to discover new drug targets and develop innovative treatments for these conditions.
Key Publications: Acta Biomaterialia, 2022, 142, 36-48; Acta Biomaterialia 2022, 140, 314-323
Therapeutic cell engineering for transplantation
Mesenchymal stem cells (MSCs) and insulin-producing islet cells are two types of cells that are commonly studied for their potential in cell-based therapies. MSCs are attractive due to their immunosuppressive properties and regenerative potential, as well as their ease of extraction and use. Islet cell transplantation is used to treat type 1 diabetes, which is caused by the destruction of insulin-secreting beta cells in the pancreas. During the transplantation, islets are isolated from a donor pancreas and infused into the liver of the recipient where they engraft and begin producing insulin.
However, a major challenge with these therapies is the poor survival of the implanted cells and the risk of immune rejection. To address this, we are developing novel bioengineering tools to enhance cell survival and function. For example, we have coated islet cells with lipids and MSCs with ECM polymers to improve their survival in human blood and silenced pro-coagulant genes to prevent thrombotic activation and enhance their survival and function. By using layer-by-layer coating or silencing pro-coagulant genes using novel nanocarriers, we can overcome immune barriers and improve the survival and function of these therapeutic cells. These strategies may lead to the development of more effective cell-based therapies for a range of conditions.
Key Publications: Biomaterials Advances, 2023, 147, 213331 , Biomacromolecules, 2021, 22 (5), 1980-1989; Biomaterials, 2013, 34, 2683-2693