Dural arteriovenous fistulas (DAVFs) are abnormal connection between extracranial arteries and intracranial veins, leading to pathological shunting of arterial blood flow to the cerebral veins that are consequently exposed to a too high flow and pressure. When this arterial flow refluxes to veins on the surface of the brain, the affected veins are at risk of rupture. DAVFs with a risk of rupture need to be treated before rupture occurs, with either endovascular embolization, microsurgery, or sometimes stereotactic radiosurgery. DAVFs are not innate but develop during life. Moreover, DAVFs are dynamic lesions that may grow or even spontaneously regress during follow-up. Our aim is to study the pathobiology of DAVFs, to better understand their untreated clinical course, treatment indications, and to possibly develop novel biological therapies that could be used as an option to more invasive procedures, especially when the DAVF does not cause an imminent risk of rupture.
* Key publications:
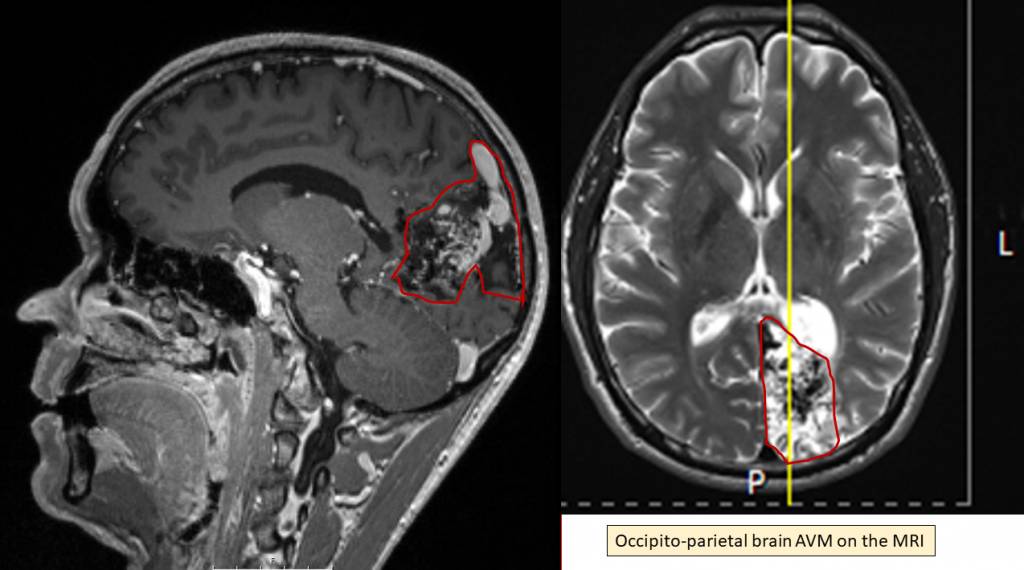
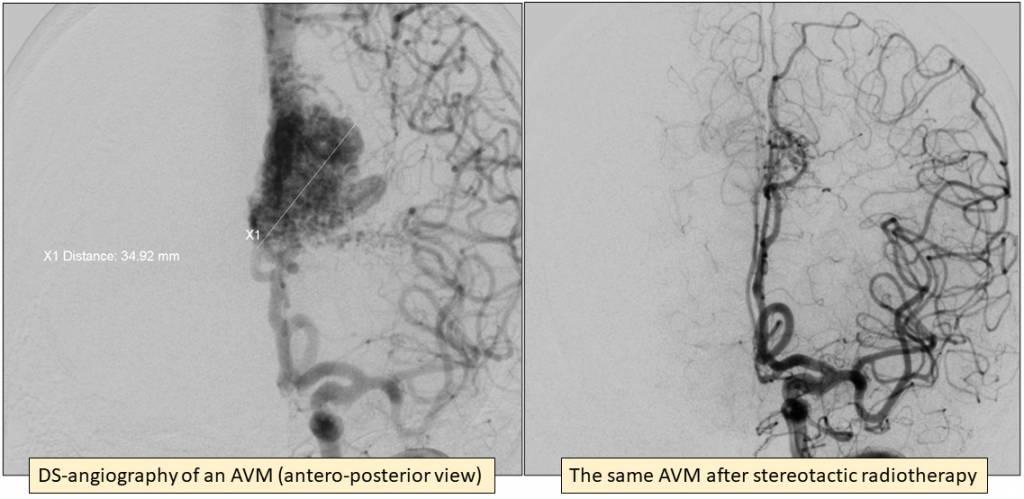
Keränen S, Suutarinen S, Mallick R, Laakkonen JP, Guo D, Pawlikowska L, Jahromi BR, Rauramaa T, Ylä-Herttuala S, Marchuk D, Krings T, Koivisto T, Lawton M, Radovanovic I, Kim H, Faughnan ME, Frösen J. Cyclo-oxygenase 2, a putative mediator of vessel remodeling, is expressed in the brain AVM vessels and associates with inflammation. Acta Neurochir (Wien). 2021 Sep;163(9):2503-2514. doi: 10.1007/s00701-021-04895-z. Epub 2021 Jun 29. PMID: 34185176; PMCID: PMC8357659.
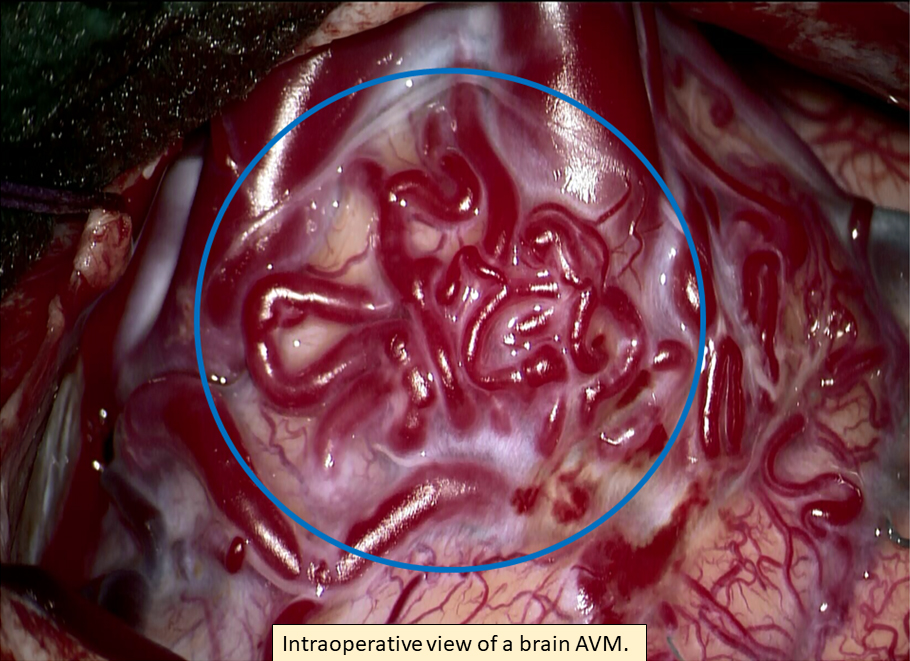
Wright R, Järvelin P, Pekonen H, Keränen S, Rauramaa T, Frösen J. Histopathology of brain AVMs part II: inflammation in arteriovenous malformation of the brain. Acta Neurochir (Wien). 2020 Jul;162(7):1741-1747. doi: 10.1007/s00701-020-04328-3. Epub 2020 Apr 18. PMID: 32306161; PMCID: PMC7295713.
Järvelin P, Wright R, Pekonen H, Keränen S, Rauramaa T, Frösen J. Histopathology of brain AVMs part I: microhemorrhages and changes in the nidal vessels. Acta Neurochir (Wien). 2020 Jul;162(7):1735-1740. doi: 10.1007/s00701-020-04391-w. Epub 2020 May 12. PMID: 32399691; PMCID: PMC7295831.
Nikolaev SI, Vetiska S, Bonilla X, Boudreau E, Jauhiainen S, Rezai Jahromi B, Khyzha N, DiStefano PV, Suutarinen S, Kiehl TR, Mendes Pereira V, Herman AM, Krings T, Andrade-Barazarte H, Tung T, Valiante T, Zadeh G, Tymianski M, Rauramaa T, Ylä-Herttuala S, Wythe JD, Antonarakis SE, Frösen J, Fish JE, Radovanovic I. Somatic Activating KRAS Mutations in Arteriovenous Malformations of the Brain. N Engl J Med. 2018 Jan 18;378(3):250-261. doi: 10.1056/NEJMoa1709449. Epub 2018 Jan 3. PMID: 29298116; PMCID: PMC8161530.
