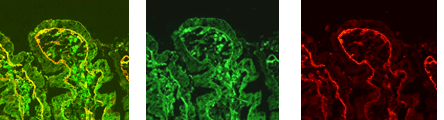
Tampere celiac researchers have been in the front-line in the development of serological tests (e.g. endomysial, TG2- and deamidated gliadin peptide antibody assays) for celiac disease. Moreover, our studies have demonstrated that celiac disease extends beyond conventional small bowel mucosal damage with crypt hyperplasia and villus atrophy that has long been used as the golden standard in diagnostics. We have identified several serological and small-bowel mucosal markers that are able to identify patients already at the early stage before development of villous atrophy. Moreover, we have shown that endomysial antibody positive patients with early stage celiac disease actually suffer from gluten-induced symptoms and that such patients benefit from gluten-free diet. Our comprehensive studies show that endomysial antibody positivity is a reliable sign of celiac disease thus implying that in many cases the diagnosis of celiac disease could be established solely by serology without invasive small bowel mucosal biopsies.
We will actively continue to work towards non-invasive diagnostic approaches and we predict that the small bowel mucosal biopsy will be replaced as the gold standard in the diagnosis of celiac disease in future, and that the diagnostic criteria will be widened towards the concept of “genetic gluten-intolerance”. Furthermore, new non-invasive diagnostics allows decentralizing diagnosis from university hospitals to secondary and primary care. Ultimately, such an approach will advance personalized and preventative medicine and lead to a considerable reduction of health care costs and save the limited resources of tertiary centers.
Our selected publications:
Kurppa K, Paavola A, Collin P, Sievänen H, Laurila K, Huhtala H, Saavalainen P, Mäki M, Kaukinen K. Benefits of gluten-free diet for asymptomatic patients with serologic markers of celiac disease. Gastroenterology 2014;147:610-7.
Ludvigsson JF, Bai JC, Biagi F, Card TR, Ciacci C, Ciclitira PJ, Green PH, Hadjivassiliou M, Holdoway A, van Heel DA, Kaukinen K, Leffler DA, Leonard JN, Lundin KE, McGough N, Davidson M, Murray JA, Swift GL, Walker MM, Zingone F, Sanders DS. Authors of the BSG Coeliac Disease Guidelines Development Group. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut 2014;63:1210-28
Kurppa K, Ashorn M, Iltanen S, Koskinen L, Saavalainen P, Koskinen O, Mäki M, Kaukinen K. Celiac disease without villous atrophy in children: a prospective study. J Pediatr 2010;157:273-80.
Kurppa K, Collin P, Viljamaa M, Haimila K, Saavalainen P, Partanen J, Laurila K, Huhtala H, Paasikivi K, Mäki M, Kaukinen K. Diagnosing mild enteropathy celiac disease: a randomized, controlled clinical study. Gastroenterology 2009;136:816-23.
Salmi TT, Collin P, Järvinen O, Haimila K, Partanen J, Laurila K, Korponay-Szabo I, Huhtala H, Reunala T, Mäki M, Kaukinen K. IgA autoantibodies against transglutaminase 2 in the small intestinal mucosa predict forthcoming celiac disease. Aliment Pharmacol Ther 2006;24:541-52.
Salmi TT, Collin P, Korponay-Szabo I, Laurila K, Partanen J, Huhtala H, Kiraly R, Lorand L, Reunala T, Mäki M. Kaukinen K. Endomysial antibody-negative coeliac disease: clinical characteristics and intestinal autoantibody deposits. Gut 2006;55:1746-1753.
Järvinen TT, Kaukinen K, Laurila K, Kyrönpalo S, Rasmussen M, Mäki M, Korhonen H, Reunala T, Collin P. Intraepithelial lymphocytes in celiac disease. Am J Gastroenterol 2003;98:1332-7.
Kaukinen K, Partanen J, Mäki M and Collin P. HLA DQ2 and DQ8 typing in the diagnosis of celiac disease. Am J Gastroenterol 2002;97:695-9.
Sulkanen S, Halttunen T, Laurila K, Kolho KL, Korponay-Szabó IR, Sarnesto A, Savilahti E, Collin P, Mäki M. Tissue transglutaminase autoantibody enzyme-linked immunosorbent assay in detecting celiac disease. Gastroenterology 1998;115:1322-8.
Collin P, Kaukinen K, Mäki M, Vuorio A. Keliakia-käypähoitosuositus.
