The oxygen deprived, ie. hypoxic conditions of ischemia were created for the cells using cardiac myocytes that were derived from induced pluripotent stem cells (iPSCs). The iPSCs had been generated from the dermal fibroblasts of a patient’s skin sample. The hypoxic conditions were achieved using the OxygenieTM platform developed by CoEBoC researchers at Tampere University.
Levosimendan significantly reduced or even abolished arrhythmias either during or after the hypoxic stress. Functionality preservation and prevention of arrhythmias are the key principles for managing cardiac ischemia. This study not only shows that the in vitro model is useful for modelling cardiac ischemia but also that there is a possible new clinical use for levosimendan. The model “could enhance the repurposing of old drugs as well as the development of novel therapies for ischemic heart disease”.
How accurately does your model represent ischemic heart disease?
That is quite a difficult question to state how accurately the model represents ischemic heart disease. Technically we can say that with the dynamics of the hypoxic system we can reach the set point value of hypoxia in four hours and maintain that for as long as needed or change the conditions if needed. We have measured oxygen levels so many times that we know how the system behaves and it is much more challenging to measure the oxygen levels with cells. Therefore, we do not need to measure that every time with cells.
How does it work fit in the current state of art?
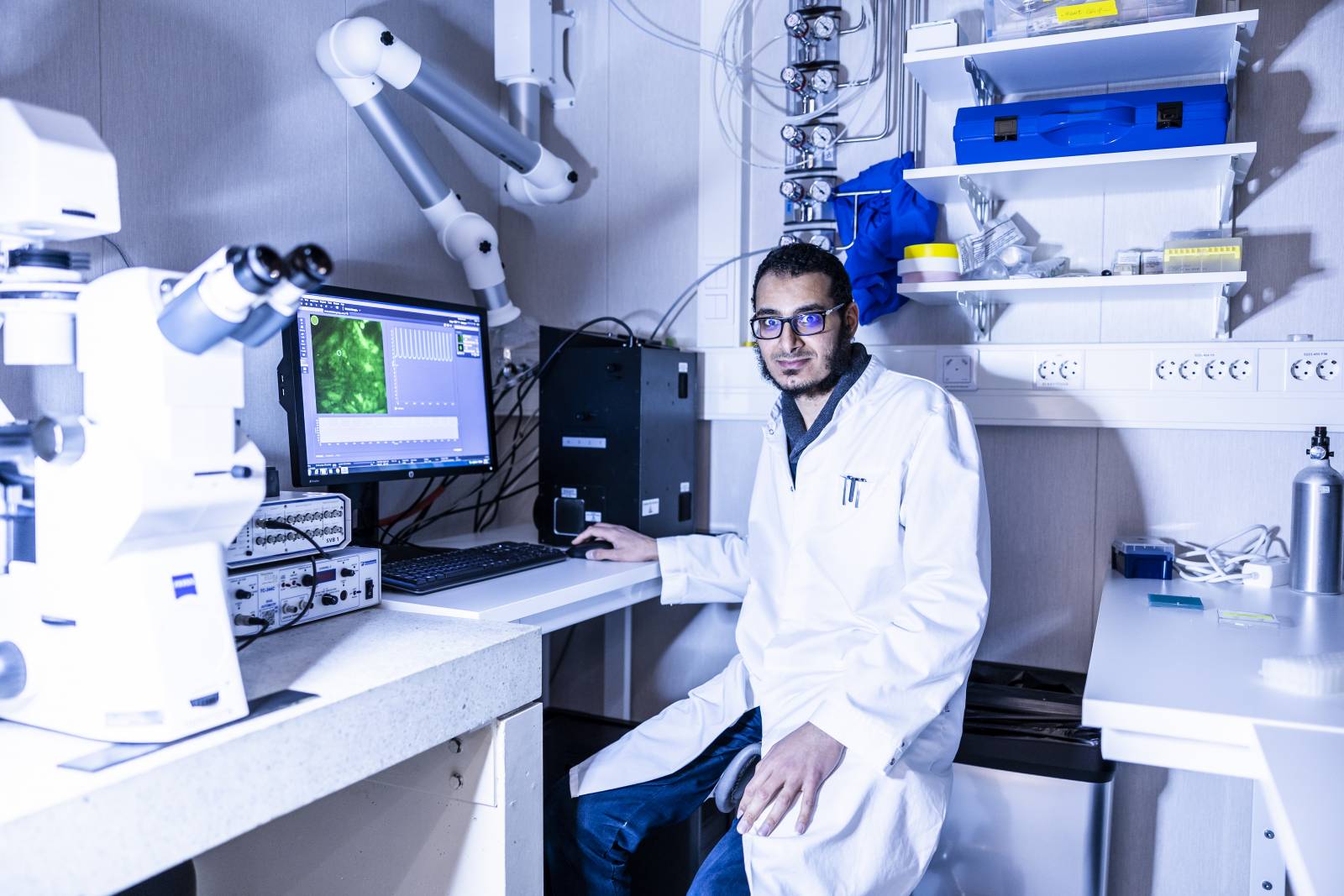
Of course, different research setups with microfluidics exist and some homemade setups as well but you can say that this setup is the only one in the world in which you can do imaging in hypoxic conditions.
What was the most interesting thing in the study?
This chip model appears to be a suitable preclinical representation of ischemic heart disease. The hiPSC-CMs showed structural changes, abnormalities in calcium transients, and beating rhythm in response to hypoxia.
Did you have any light-bulb moments during the project?
Quite a momentous addition to the plan was to test the levosimendan drug which was brought up by the group leader during a group meeting. The drug testing became an especially important part of the project and had interesting results.
How was the planning and timeline of the project?
I personally expected the project to be done in a year, but it went on for two years. This was due to poor cell behavior during the differentiation process and the corona situation at the time.
The planning of this project was quite quick, and this was because the things needed were found in-house (in CoEBoC). It was a collaboration between two in-house research groups (Heart research group and the Micro & NanoSystems research group), making communication and working together easy and fast.
Read the full article here: Cardiac Ischemia On-a-Chip: Antiarrhythmic Effect of Levosimendan on Ischemic Human-Induced Pluripotent Stem Cell-Derived Cardiomyocytes