Researchers from the Faculty of Medicine and Health Technology (MET) at Tampere University have successfully created a cell culture platform that allows two cultivated vascular networks to interconnect. The blood vessels in these networks are equivalent to human capillaries in size and structure, facilitating the study of human capillary networks in a laboratory setting. Their research paper was published in Scientific Reports on 2 October 2024.
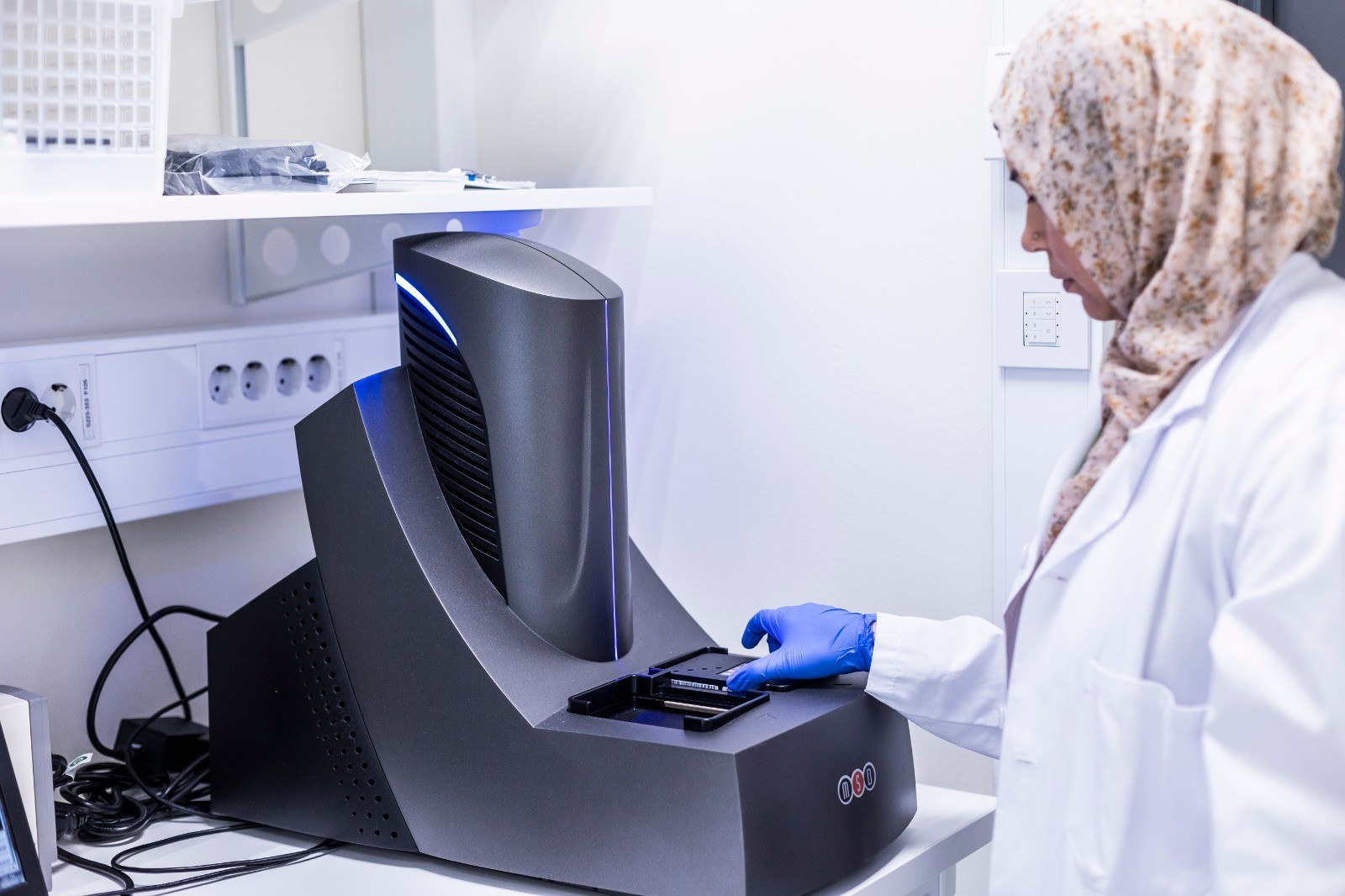
“The generation of two distinct, interconnected 3D microvascular networks marks a significant step forward in our research. Now we can incorporate cells found in different types of tissue around these interconnected vascular networks – such as hepatocytes from liver tissue and adipocytes from fat tissue – to study cellular interactions in vascularized tissues,” says Alma Yrjänäinen. She is working on her PhD within the Centre of Excellence in Body-on-Chip Research at Tampere University.
 Organ-on-chip (OoC) technology combines microfabrication techniques and cell biology to facilitate the study of tissue functions. OoCs replicate the complex microenvironment of human tissue by incorporating either gravity-driven or pump-assisted fluid flow through miniaturised tissue, mimicking the natural forces of blood flow. Neurons and blood vessels can also be integrated into these models.
Organ-on-chip (OoC) technology combines microfabrication techniques and cell biology to facilitate the study of tissue functions. OoCs replicate the complex microenvironment of human tissue by incorporating either gravity-driven or pump-assisted fluid flow through miniaturised tissue, mimicking the natural forces of blood flow. Neurons and blood vessels can also be integrated into these models.
OoCs can substantially reduce the costs of drug discovery, with experts estimating a potential reduction of up to 25%. National healthcare systems could also benefit from the adoption of OoCs. However, further progress is needed before these visions become a reality.
“Imagine that in the future, a single blood sample could unlock a personalised treatment for your hypertension. Stem cells derived from your blood could be used to create a vascular network in a laboratory setting. This network could then be used to test which hypertension drugs available on the market would be most suitable for your cells, helping to avoid drugs that would be ineffective or even harmful to you,” Yrjänäinen says.


 Juliana von Wendtin Säätiön juhla-apuraha Hanna Vuorenpäälle eläinystävällisten vasta-aineiden testaamiseen
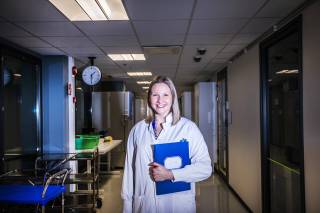
Juliana von Wendtin Säätiön juhla-apuraha Hanna Vuorenpäälle eläinystävällisten vasta-aineiden testaamiseen See what motivates our Postdoctoral research fellow Hanna Vuorenpää to develop 3D human tissue models
See what motivates our Postdoctoral research fellow Hanna Vuorenpää to develop 3D human tissue models Great success for Alma Yrjänäinen in pitching her PhD thesis
Great success for Alma Yrjänäinen in pitching her PhD thesis